Aldweib及同事评价既往血运重建的无症状患者心肌灌注成像和后续血运重建的益处。6750例既往血运重建患者接受心肌灌注闪烁显像(MPS),769例有缺血且无症状,15%进行血运重建。接受血运重建治疗与接受药物治疗的缺血患者相比,全因死亡无差异。在校正基线特征、既往血运重建类型、MPS数据和倾向评分后,只有年龄和高胆固醇血症,而非血运重建,与死亡率相关。既往血运重建且MPS提示,可诱导缺血的无症状患者未从再次血运重建中获得生存获益(图3)。
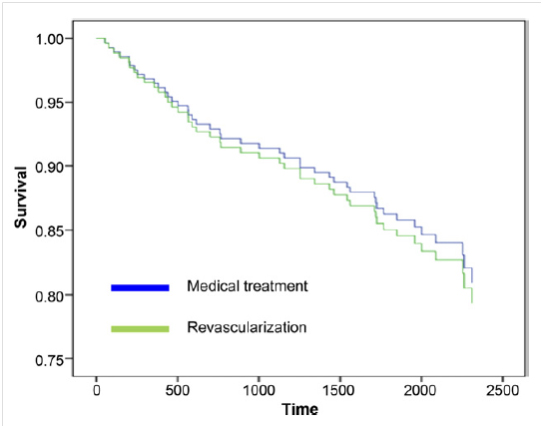
图3. 校正年龄、性别、射血分数的倾向配对患者生存率
J Am Coll Cardiol.2013;61(15):1616-1623.
特约点评
血运重建后无症状患者常规负荷核素显像及随后的血运重建
Routine Nuclear Stress Testing and Subsequent Revascularization in Asymptomatic Patients Following Coronary Revascularization
Zaher Fanari, Sandra Weiss, William S Weintraub.
Christiana Care Health System, Newark, DE,美国
Myocardial perfusion scintigraphy (MPS) can stratify risk in symptomatic and asymptomatic patient. However, the benefit of such testing to guide subsequent revascularization in patients with stable coronary disease and asymptomatic patients is uncertain. Moreover, MPS testing in patients’ post-revascularization remains widely utilized, justified by the assumption that post-revascularization ischemia is an adverse prognostic finding regardless of symptoms, and that repeat revascularization would be of benefit in reducing subsequent events, in particular myocardial infarction (MI) or death. However, there is little evidence supporting such a practice. In the April issue of the Journal of the American College of Cardiology, Aldweib et al. compared the survival of asymptomatic patients with MPS-identified post-revascularization ischemia who subsequently underwent repeat revascularization in addition to optimal medical therapy (OMT) versus OMT alone. The authors performed a retrospective analysis of 769 patients, in whom 115 (15%) underwent repeated revascularization in response to identified ischemia. The study demonstrated no difference in the primary endpoint of all-cause mortality between the revascularization and OMT groups (18.3% vs. 19.1%, P=0.84), despite adjustment for degree of MPS ischemia (mild vs. moderate-severe), degree of scar, and left ventricular ejection fraction using propensity score methods. The authors concluded that routine MPS and subsequent intervention in patients with post-revascularization silent ischemia did not offer survival benefit.
This study should be praised in that it is the first to evaluate post-revascularization patients with silent ischemia by MPS, a population that heretofore has not been studied and where questions regarding management certainly remain. This lack of data on reflexive stress imaging post-revascularization is highlighted by the disparity in current practice guidelines and appropriateness statements on this issue. Notably, the 2011 Guidelines on Percutaneous Coronary Intervention (PCI) recommends against routine testing, while the 2009 Appropriate Use Criteria for Cardiac Radionuclide Imaging suggests that stress testing 2 years following PCI and less than 5 years following CABG is considered uncertain, leaving room for individual interpretation of appropriateness in patient who remain asymptomatic. Although revascularization of identified ischemia in increasingly symptomatic, medically optimized patient is well established and appropriate, further intervention on previously revascularized individuals with residual silent ischemia is based largely on extrapolation from studies performed in patients with chronic stable angina or asymptomatic, but previously unrevascularized individuals. These patient populations are quite unique from that which was studied here and whose study findings were inconsistent.
Early data supporting the benefit of revascularization of residual ischemia in stable CAD came from a series of observational and post-hoc analyses. Hachamovitch et al. found that patients with significant ischemia by MPS realized a survival benefit from early revascularization. Further, data from the nuclear substudy of the COURAGE trial supported this, demonstrating that patients with moderate-severe pre-treatment ischemia by MPS (>10% myocardium) had a greater reduction in ischemic burden and saw an early decrease in death and MI. However, the benefit noted in these studies was more recently put into context by the long-term results of the COURAGE nuclear substudy that revealed no difference in death or MI, regardless of the degree of ischemia, therefore calling this practice in stable CAD into question. In addition, a COURAGE cost effectiveness analysis found that revascularization in stable CAD was associated with increased cost without significant gain in life-years or quality-adjusted life-years.
Data surrounding revascularization of identified silent ischemia comes from the ACIP trial, SWISS Ⅱ trial and the silent ischemia subgroup of COURAGE. The former two involved patient with either angiographically documented coronary artery disease or non-revascularized recent MI and silent ischemia by stress testing, showing reduced major adverse cardiac events in those who underwent PCI when compared to OMT. However, the more contemporary silent ischemia subgroup of COURAGE, which more closely reflects current PCI and OMT strategies, demonstrated no significant differences in the primary end point of death or MI between PCI and OMT in patients with largely unrevascularized asymptomatic ischemia. The authors did note, however, a non-significant trend toward fewer deaths in the PCI group (5% vs. 11%, P=0.12), suggesting an issue of underpowering to demonstrate this potential benefit. Therefore, not only do questions remain about the appropriateness of revascularization in these patient subgroups, but extrapolating to patients with residual silent ischemia post-revascularization is even more problematic. The study by Aldweib et al. is the first to isolate this latter unique population and shed light on this important management question.
However, there are several limitations to the study. First, only 15% of the study population underwent revascularization based on MPS findings. Although suggested to be appropriately powered, is it a minority of the total population enough to draw conclusions? Second, it is unclear whether the location of ischemia could impact the findings as there are data demonstrating mortality benefit from left anterior descending, but not from left circumflex or right coronary artery revascularization. These data were not reported and the study numbers would be too small to demonstrate such an effect. Third, it is unclear what type of revascularization (PCI vs. CABG) was used for the subsequent revascularization as that might impact the survival. Finally and importantly, the retrospective observational design of the study is subject to selection bias and unmeasured confounding that propensity score analysis may help to minimize but cannot completely eliminate. Prospective, randomized data on the usefulness of routine testing after revascularization and subsequent PCI for silent residual ischemia is limited and necessary to fully elucidate this issue, although such a study most likely would prove logistically and monetarily prohibitive.
Despite these issues, the results presented by Aldweib et al. make a compelling argument that routine stress testing and subsequent intervention in asymptomatic patients following coronary revascularization offers no clinical benefit. It is the opinion of the authors that such a strategy is unlikely to add benefit and is associated with increased cost and poor utilization of much needed resources. Until prospective data show a benefit from such a strategy, routine stress testing in asymptomatic patient post revascularization remains of unproven benefit.
心肌灌注闪烁显像(MPS)可对有症状和无症状患者危险分层,但应用这项检测指导稳定性无症状冠心病患者血运重建的获益不明。基于血运重建后心肌缺血提示预后不良、再次血运重建可减少心肌梗死或死亡事件的假设,MPS在血运重建后被广泛使用,但缺乏证据支持这种实践。这项回顾性分析首次评估血运重建后MPS提示无症状性缺血患者,值得称赞。由于缺乏研究证据,对这类患者管理的指南推荐不一。2011年经皮冠状动脉介入治疗(PCI)指南不推荐常规MPS检查,而2009年放射性核素显像规范对PCI后2年和旁路术后5年之内负荷检查持不确定意见。
这项研究的局限在于:①仅15%的研究对象根据MPS结果进行血运重建,结果是否能反映整体研究人群?②缺血部位是否影响结果?有数据显示,左前降支血运重建可能获益,左回旋支和右冠状动脉则不能。③研究中采取何种血运重建,PCI或旁路手术?④这是一项回顾性分析,倾向评分不可能完全消除选择偏倚和未测量的混杂因素。
尽管如此,这项研究结果仍提示,血运重建后无症状患者常规负荷核素显像及其后的再次血运重建并无临床获益。作者认为,这种临床策略将增加费用,占用有限医疗资源。
[下一页] [1] [2]