James Lee, Zhen Qian, Gustavo Vazquez, Reynaria Pitts, Shelley Holt, Vivek Rajagopal, Mani Vannan, Sarah Rinehart 美国Piedmont心脏研究所
Sarah Rinehart 美国Piedmont心脏研究所心脏病学家,主要研究领域是心脏影像。她积极参与心脏研究,例如颈动脉和冠状动脉粥样硬化的区域性研究和预防,尤其是使用心脏CT / MR。
经导管主动脉置换/植入术(TAVR/TAVI)血管通路并发症较多,并可能增加瓣周漏。使用多模立体成像有助于解决这个问题。Bloomfield等指出TAVR术前影响评估目标:①测量主动脉瓣环;②测量瓣叶长度和钙化;③定位冠状动脉开口;④识别其他可能影响植入的因素; ⑤进行术前计划。
经胸超声心动图(TTE)可对主动脉瓣狭窄和选择外科或TAVR方法做出初步评估。尽管存在操作者依赖和只能评估瓣环的1维等缺陷,在PARTNER试验中使用TTE仍取得成功。经食管超声(TEE)在植入瓣膜时非常重要。多排CT(MDCT)可以评估主动脉瓣环,主动脉根,瓣膜结构、钙化和评估路径,其主要缺点是碘对比剂的潜在危害。
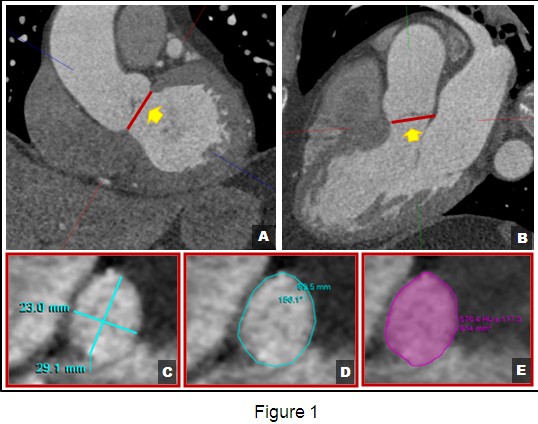
为选择TAVR植入瓣膜的合适尺寸,有必要评估主动脉瓣环、主动脉窦尺寸,冠状动脉开口与瓣环的距离,窦管连接处和瓣环上40 mm处的主动脉直径。MDCT对于评估瓣环的椭圆结构优于TTE。使用MDCT测量瓣环,图像应当在两个垂直平面排列,采集3个瓣膜插入点。在心室收缩期进行测量。使用以下基本方法:①测量瓣环最大和最小直径的平均值;②测量瓣环的圆周长;③计算瓣环面积。使用多模立体成像需要对尺寸进行调整,因为TTE测量的瓣环比TEE小1 mm,比MDCT小1~1.5 mm。
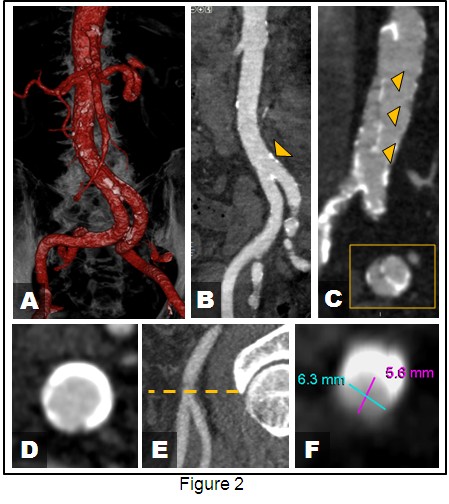
MDCT可用来评估血管通路,排除不适合作为血管入路的髂-股动脉,如直径过小、钙化、成角等问题。MDCT还能对其他动脉与动脉瘤的情况进行评估。
Aortic stenosis is the most common valvular disease of the elderly. The natural history of symptomatic aortic stenosis is extremely poor and approximately 50% of patients will not survive past two years. Aortic valve replacement improves the long-term survival in patients with aortic stenosis. However, despite benefits of surgery, approximately 1/3 of elderly patients are deemed not to be surgical candidates.
Transcatheter Aortic Valve Replacement / Implantation (TAVR/TAVI) was first introduced in 2002 and is rapidly becoming an accepted intervention for the treatment of high risk patients with severe aortic stenosis. Compared to standard therapy, TAVR achieved a 20 percentage point reduction in the rate of all-cause mortality at 1 year in patients who could not undergo surgery. As an alternative therapy, TAVR has been found to perform similarly in terms of death rate from any cause, symptom reduction, and valve hemodynamic improvement at 2 years compared to surgical aortic-valve replacement. The two devices currently available are the Edwards SAPIEN Transcatheter Heart Valve and the Medtronic CoreValve. The SAPIEN valve was approved by the FDA October 2012 and the CoreValve is currently only available in clinical trials. At this time, TAVR prostheses have been implanted using transfemoral, subclavian, transapical and direct aortic approaches.
However, TAVR is not without its challenges and vascular access complications are common with rates between 6.3%~30.7%. In addition, TAVR treated patients have greater frequency of paravalvular regurgitation than surgically treated patients and even mild paravalvular regurgitation is associated with increased late mortality. Many of these issues can be mitigated with multi-modality imaging. Bloomfield et al. have outlined the goals of pre-planning for TAVR with multimodality imaging as follows: ①measuring aortic annulus size; ②measuring leaflet length and calcification; ③locating the coronary ostia; ④identifying other features that might interfere with successful implantation; and ⑤contributing to pre-procedural planning.
Trans-thoracic echocardiography (TTE) is a valuable tool in the pre-procedural planning of TAVR. It is the basic step of assessing severity of aortic stenosis and thus candidates for surgical or TAVR intervention. However, the image acquisition is often operator dependent and can only assess 1 dimension of the aortic annulus. Despite this limitation, there was great success with the PARTNER trial using TTE for the basis of sizing of the valve. Transesophageal echocardiography (TEE) is essential during implantation of the valve and holds promise for evaluation of the aortic
annulus.
Multi-detector Computed Tomography (MDCT) is evolving as a powerful complementary test for the pre-procedural planning of TAVR. It is hoped that improvements in prosthesis sizing will reduce complications during implantation, including paravalvular leak. Major indications for MDCT prior to TAVR include evaluation of the aortic annulus, aortic root, valve structure, calcification and access route. The main drawback of MDCT is exposure to potentially nephrotoxic iodinated contrast agents. Radiation exposure is of less concern given the advanced age of patients undergoing TAVR.
The technical aspects of acquiring measurements for TAVR with MDCT, as well as the standard measurements obtained, are well documented in the SCCT expert consensus document. Images of the valve should be acquired with EKG gating using a slice thickness of <1.0 mm. Contrast bolus should be timed for the ascending aorta similar to coronary CTA.
For the appropriate sizing of TAVR prosthesis, it is important to assess the aortic annulus size, the size of the sinuses of Valsalva, the coronary ostia distance from the annulus, the size of the aorta at the sino-tubular junction and 40 mm above the annulus. Correct annular sizing is critical for the pre-procedural planning of TAVR as under-sizing of the prosthesis can contribute to paravalvular aortic regurgitation as well as valve embolization. Over- sizing of the prosthesis to the aortic annulus has been associated with aortic root rupture. In addition, the correct positioning of the valve is also important because incorrect positioning can lead to increased paravalvular aortic regurgitation or place the coronary ostia at risk for occlusion.
There are several challenges to correctly assessing the aortic annulus. The aortic annulus is known to be an oval shaped, virtual ring formed by the joining of basal attachments of the aortic valvular leaflets. MDCT is much better suited for measuring the elliptical structure of the annulus compared to TTE because TTE systematically underestimates the major dimension of the annulus. The annulus should also be measured during systole because it undergoes conformational, pulsatile changes during the cardiac cycle. Utilizing diastolic measurements risks under-sizing of the prosthesis.
In order to measure the annulus on MDCT, the images should be lined up in two orthogonal planes and capture all 3 valve insertion points. Measurements should be performed in ventricular systole (20%~45% of the RR interval). Annular measurements are completed using three primary methods: ①Measurement of the average of the major and minor annulus diameters. D=(Dmax+Dmin)/2; ②Measurement of the perimeter with assumption of circularity of annulus. D=Perimeter/pi; and ③Planimetry of the area with assumption of circularity of annulus [D=2*sqrt(A/pi)]. However, with the use of multimodality imaging, there may be a need to “adjust the sizing of the prosthesis” because annular assessment by TTE is on average 1mm smaller than TEE, which is approximately 1~1.5 smaller than MDCT.
In terms of vascular access, MDCT easily delineates unfavorable ilio-femoral anatomy for TAVR such as a minimal luminal diameter of the common iliac, external iliac, or common femoral artery of less than 8 mm; presence of greater than 60% circumferential calcification at the external-internal iliac bifurcation; and severe angulation (<90 degrees) between the common and external iliac arteries. It is also important to obtain similar information regarding the subclavian arteries, ascending aorta, aortic arch, and descending aorta depending on the route of access planned. Additional aortic considerations include aneurysm and dissection formation.
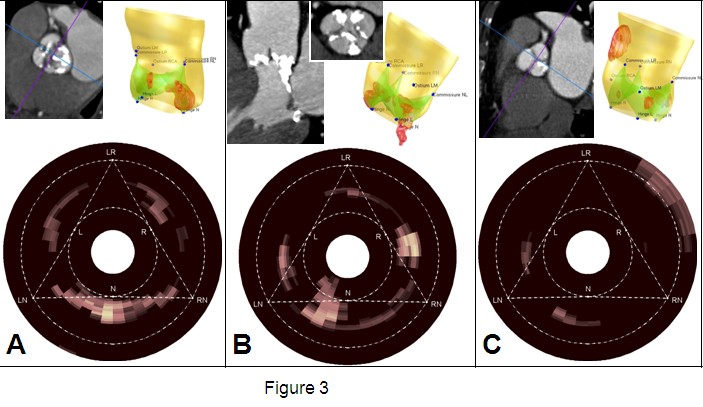
There are exciting developments in pre-procedural planning with TAVR. At our institution, there is active development of an automated 3D model of the aortic root and aortic valvular calcification maps, which hold great promise in TAVR prosthesis sizing.
[下一页] [1] [2] [3]